 |
Interesting Articles about Popular Topics |
|
|
Kathleen E Bachynski[1], Michelle Canham-Chervak[1], Sandra A Black[2], Esther O Dada[1], Amy M Millikan[2], Bruce H Jones[1] March 7, 2012 Objective
Methods
Results
Conclusions
Suicides among US Army personnel have risen steadily since 2004.[1] Historically, suicide has been reported as one of the leading causes of death in the US military,[2 ,3] although military suicide rates have been lower than rates of comparable non-military populations.[4] Military suicide rates, however, are now surpassing those among comparable civilian populations. In 2008, estimates of the rate of suicide among active duty soldiers in the regular army, army reserve and army national guard began surpassing the suicide rate among US civilians with similar demographics.[1 ,5] Whereas civilian rates adjusted to the gender structure of the US Army (younger age and higher percentage male) have remained approximately 18 per 100,000, army rates have increased to over 20 per 100,000.[5-7] In order to address this emerging public health problem, modifiable risk factors for suicide must be identified. Further understanding of the epidemiology of suicide and associated risk factors in the army would facilitate prevention and reduction efforts. Suicide is complex and multifactorial, with a host of potential and interacting risk factors that have been examined in both the civilian and military literature. Of these, mental health disorders are among the most consistently reported and extensively researched,[8-12] and may be of particular relevance to the recent increase in suicide rates in the US Army. Individuals with major depressive disorder and bipolar disorder are highly vulnerable to suicidal behaviour; in more than half of all suicides, depression has been shown to be a significant risk factor.[13 ,14] Anxiety disorders, psychotic disorders, as well as alcohol and illicit drug abuse, have been found to be associated with suicides, as have personality disorders, particularly schizoid, borderline and narcissistic disorders.[15-22] Adjustment disorder and post-traumatic stress disorder (PTSD) are frequent mental health diagnoses among military personnel that have been associated with suicide.[23-26] The risk of suicide is particularly elevated in the presence of comorbid mental and behavioural health disorders.[10 ,27] The purpose of this analysis is to use Department of Defense (DoD) administrative and medical surveillance data to provide a preliminary epidemiological assessment of the association of mental disorders with suicide during the years 2007-8. This observational analysis is intended to generate hypotheses and promote further study of the public health problem of suicide in the US military. In addition, this paper documents historical trends (years 1977-2008) in the rates of suicide and recent trends (years 2000-8) in the rates of mental illness among soldiers in the US Army. A final objective was to assess changes in suicide rates that might be associated with involvement in large combat operations. The data for this analysis came from the Army Behavioural Health Integrated Data Environment, which was established in 2009 by the US Army Public Health Command Behavioural and Social Health Outcomes Programme. This suicide registry consolidates army suicide data from sources including the Defense Casualty Information Processing System, the Department of Defense Manpower Data Center, and the Defense Medical Surveillance System,[28] an administrative database that captures and maintains information relevant to clinical encounters, including diagnoses from medical providers at the time treatment is received. Analyses were restricted to suicides that occurred among soldiers on active duty in the US Army during 2007 and 2008 (the most recent 2-year period for which complete data were available at the time it was obtained in August 2009). Medical data were available only for soldiers on active duty (as it is maintained in active DoD administrative databases); US Army National Guard and Reserve soldiers typically do not serve full time and do not receive most of their medical care in military treatment facilities. Data for suicides included demographics, deployment history and mental health disorders that were diagnosed and treated in military medical facilities or paid for by the military health system. These data were initially obtained in August 2009[29] and were updated in June 2010. Potential cases of suicide were first identified in the Defense Casualty Information Processing System. If confirmed as suicides by the Armed Forces Medical Examiner's Office, they were included as suicide cases in this analysis. Medical encounter measures, including mental health diagnoses, reflect the time period from entry into service to the time of death, discharge from service, or end of the study period (December 2008). The total number of soldiers who had ever deployed versus never deployed was obtained from the Armed Forces Health Surveillance Center. Comparable data for denominator and risk factors for the army as a whole were obtained from the Defence Medical Epidemiology Database, a web-based application that provides remote access to data contained within the Defense Medical Surveillance System via user-defined queries.[30] All queries took place in August 2009 and were restricted to active duty army personnel from 2007 to 2008. Ninety four per cent of medical encounters for mental health disorders were ambulatory visits, and most (76%) soldiers who were hospitalised for a mental health disorder had the same or a similar diagnosis on one or more outpatient visits before their hospitalisation. Ambulatory data were thus used for the calculation of rates and relative rates of suicide risk associated with specific mental health disorder categories. Results reflect mental disorders diagnosed from January 2007 to December 2008 and were restricted to primary diagnosis and first occurrence per person only. Secondary diagnoses and comorbid mental disorders were not included due to the inability to ascertain the onset and timing of diagnoses from the administrative data. In addition, US Army rates of suicide during the years 1977-2008 were obtained from US Army G-1 (Personnel) in October 2009 in order to assess historic trends. The proportion of suicides in 2008 that may be attributed to post-2003 events (ie, attributable risk) was estimated by comparing the expected rate of suicide in 2008 (based on previous years) with the actual rate of suicide in 2008. MeasuresDemographic characteristics included gender, age, race/ethnicity and marital status. Age was divided into three categories: 18-24, 25-34 and 35 years or older. Race/ethnicity included Caucasian, African-American and other (eg, Native American, Asian/Pacific Islander and Hispanic). Marital status was categorised into single, married and other (which, due to small numbers, includes separated, divorced and widowed). Military rank was categorised into lower enlisted (E1-E4), senior enlisted (E5-E9) and officers. Deployment history included ‘ever’ or ‘never’ deployed to combat. Mental health diagnoses were categorised as ever or never diagnosed, and were grouped into four diagnostic categories: Mood disorders, anxiety disorders, substance-related disorders and other disorders, which included adjustment disorder, personality disorders and psychotic disorders. Determination of disorders was based on International Classification of Disease, version 9, clinical modification (ICD-9-CM) codes[31] recorded in the administrative datasets and the Defense Medical Surveillance System. These groupings were adapted from the mental health and substance abuse clinical classifications developed by the Agency for Healthcare Research and Quality.[32] Table 1 shows the diagnostic categories and specific mental health disorders that were assessed, as well as the ICD-9-CM codes associated with each specific disorder. 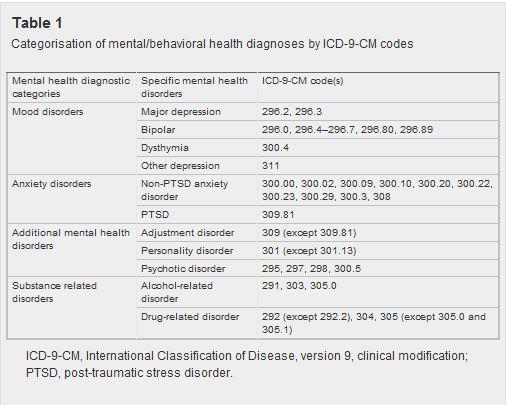
Descriptive statistics on demographic and mental health risk factors and the relative burden of suicide and mental health disorders in the US Army (rates and counts) for 2007 and 2008 were assessed and compared using relative risks (RR) and 95% confidence interval (CI). In order to assess changes in suicide rates that coincided with increased involvement in large combat operations, we used a linear regression of suicide data from 1977 to 2003 (the point when the major commitment of US troops to the Iraq war started) to project the expected rate of suicides for 2008. The observed 2008 rate was compared with the estimated rate to estimate ‘attributable risk’ for that year. The equation for ‘percent attributable risk’ is (rate in exposed)-(rate in unexposed)/(rate in exposed), where ‘unexposed’ represents the expected suicide rate given peacetime conditions and ‘exposed’ is the actual suicide rate among army soldiers following major deployment to combat operations.[33] Due to small sample sizes, data for both years were combined to assess risk factors for suicide deaths among active duty army personnel. Chi-square tests and relative rates of suicide were calculated for each category and compared across groups. Two-by-two tables were constructed using Defense Casualty Information Processing System data to identify suicide cases (numerators) and Defense Medical Surveillance System data to identify non-suicide cases (denominators) to calculate RR. Rates, RR and 95% CI were validated using the online calculator for comparing person-time rates available at: http://www.openepi.com.[34] Statistical significance was set at a=0.05. While rates based on counts smaller than 20 are generally considered statistically unreliable,[35 ,36] they are reported as initial estimates and for subsequent hypothesis generation. Rates and RR are not reported for cell sizes less than five. US Army suicide rates nearly doubled from 2004 to 2008, in contrast to the previous slightly downward trend observed since 1977. Figure 1 highlights these trends and compares actual 2004-8 rates of suicide among active duty soldiers with projected 2004-8 rates. Projected rates were based on the assumption that the declining trend of recorded suicide rates observed for the years 1977-2003 would have continued to 2008. The trend line based on 1977-2003 suicide rates and projected to 2008 shows a slightly decreasing trend among the active duty army, whereas the trend line based on actual suicide rates for the years 2004-8 shows an increasing trend. Lines 2 standard deviations (SD) above and below the 1977-2008 trend line provide further statistical context for the temporal variation in suicide rates. Over the 27-year period from 1977 to 2003, no points fell beyond 2 SD of the expected trend. In the following 5-year period (2004-8), however, the rates for 2006, 2007 and 2008 were more than 2 SD above the expected range. 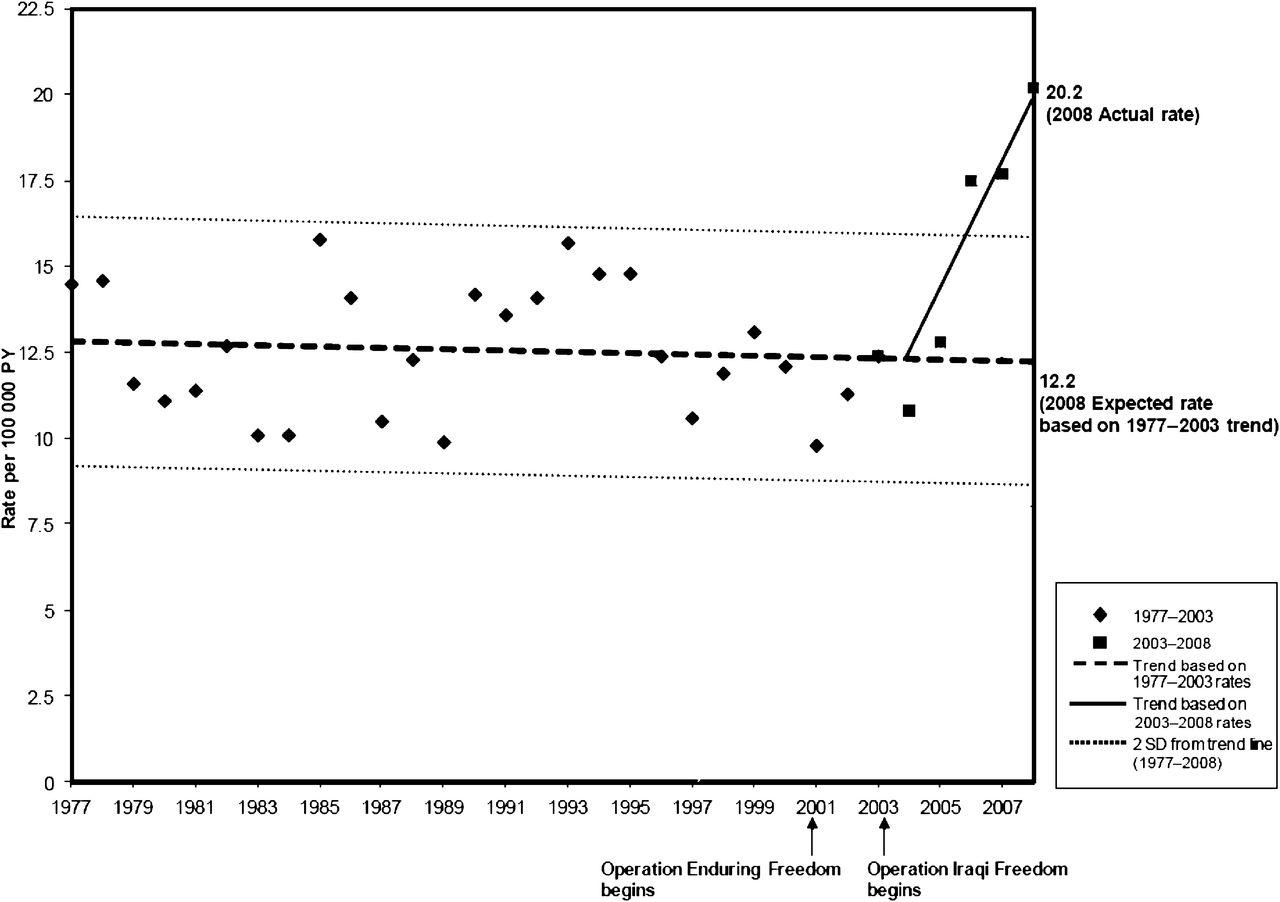
Figure 1. Active duty US Army suicide rates, 1977-2008. (Data source: US Army G-1.) Comparing the actual 2008 suicide rate (20.2 per 100,000 person-years) with the expected 2008 suicide rate (12.2 per 100,000 person-years) results in an attributable proportion of 0.39 (95% CI 0.27 to 0.52). This suggests that an estimated 39% of suicides that occurred in 2008 may be associated with post-2003 military events. The 95% CI around the point estimate gives an estimated range of 27-52% of deaths by suicide associated with post-2003 military events. In relation to mental health disorders, the combined rates of ambulatory visits for the disorders examined nearly doubled from 2000 to 2008. This increase was steady and sharpest in the period 2003-8, nearly doubling from a rate of 116 per 1000 in 2003 to 216 per 1000 person-years in 2008. Figure 2 illustrates this trend in rates by the type of mental disorder. A similar trend was seen in hospitalisations, with an overall increase from 7.4 per 1000 in 2003 to 14.0 per 1000 in 2008. 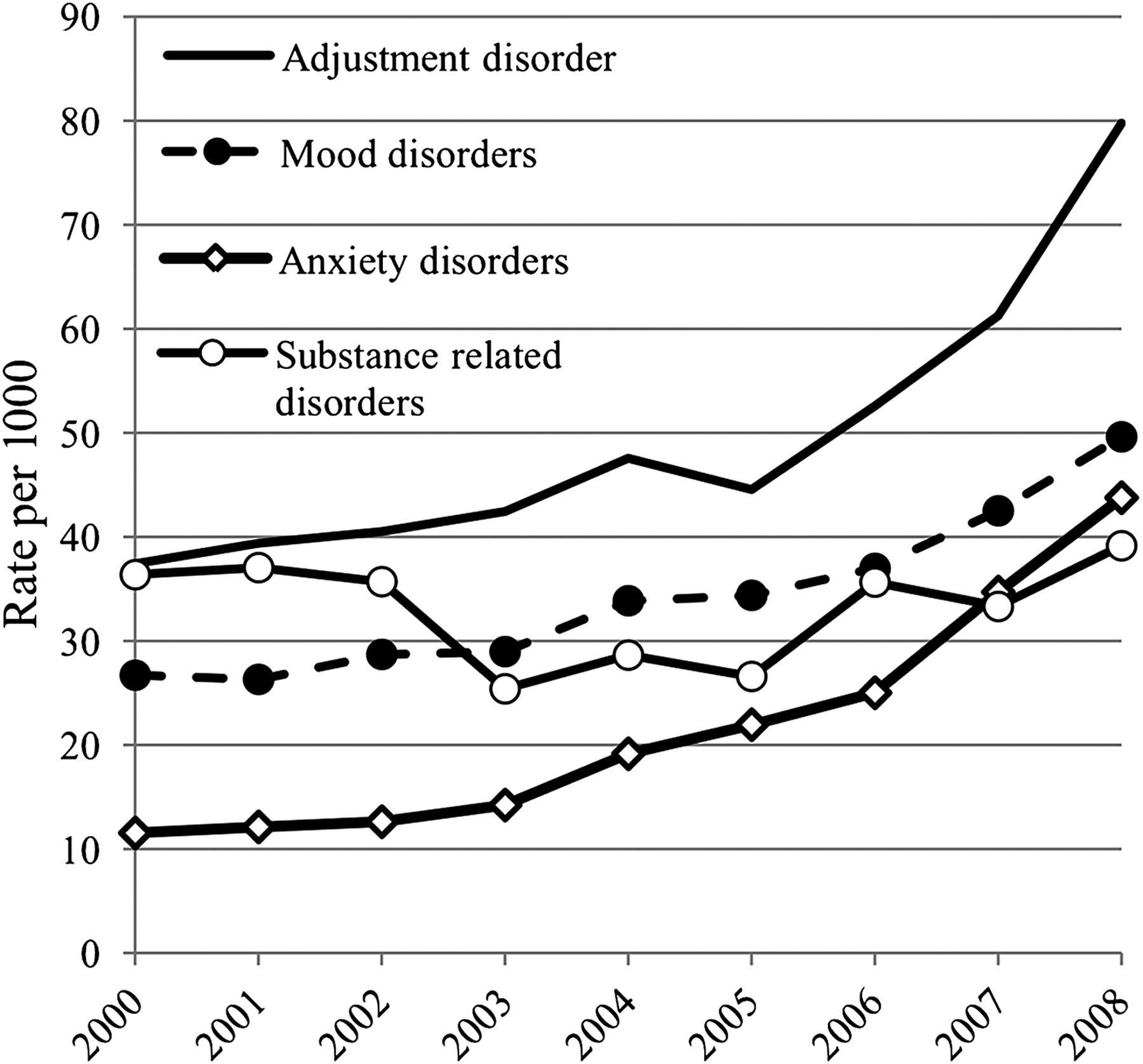
Figure 2. US Army rates of mental health disorders, ambulatory visits 2000-8. (Data Source: Defense Medical Surveillance System; diagnoses based on primary diagnosis, first occurrence only.) Demographic characteristics and their associations with suicide A total of 255 active duty soldiers committed suicide in 2007 and 2008 (115 in 2007 and 140 in 2008). Table 2 presents the distribution of demographic characteristics for this group of individuals. Suicides were predominantly male (95%), 18-24 years old (45%) and Caucasian (73%), married at the time of death (59%) and lower enlisted (54%). Almost 69% had been deployed at least once to combat theatre. Table 2 also displays the RR associated with each of the demographic and military characteristics. Male gender was significantly associated with suicide, although it should be noted that the rates are unstable for women due to small numbers. Soldiers aged 25-34 years and African-American individuals were at a significantly lower risk of suicide. The risk of suicide did not differ between soldiers who were married and those who were single. Among the military ranks, the lower enlisted (E1-E4) had a significantly higher rate of suicide than officers. The RR for suicide was higher among those ever deployed compared with those never deployed, but the difference was not statistically significant. 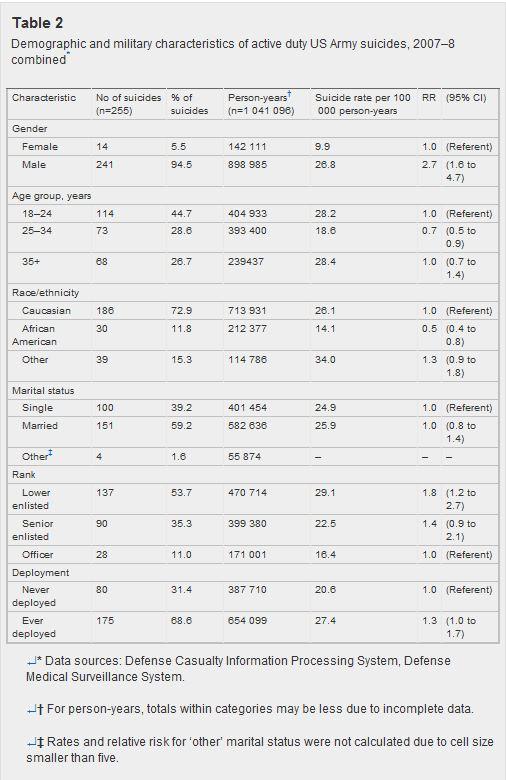
Mental health disorders and their associations with suicide Of the 255 suicide cases, 44 (17%) had a previous hospitalisation from January 2007 to December 2008, and 128 (50%) had a previous ambulatory visit for a mental health disorder during this period. Those with a hospitalisation for a mental disorder were 15.5 (95% CI 11.2 to 21.5) times more likely to commit suicide compared with those who were not hospitalised for any mental health disorder during this time period. Those with an ambulatory visit for a mental disorder were 3.9 (95% CI 3.0 to 4.9) times more likely to commit suicide compared with those who did not have an ambulatory visit for a mental health disorder during this time period. Table 3 shows the distribution and RR of suicide associated with specific mental health disorders for 2007-8 combined. It should be noted that an individual could have more than one diagnosis of a mental disorder. All the selected mental disorders were significantly associated with death from suicide (X2 p value <0.001). Among the mood disorders, the RR for suicide among those with an ambulatory visit for dysthymia was 11.5 (95% CI 7.0 to 18.8), 6.5 (95% CI 4.1 to 10.1) for major depression, 5.5 (95% CI 2.4 to 12.3) for bipolar disorder, and 7.8 (95% CI 5.6 to 11.1) for other depressive disorders, in comparison with soldiers who did not have such diagnoses. 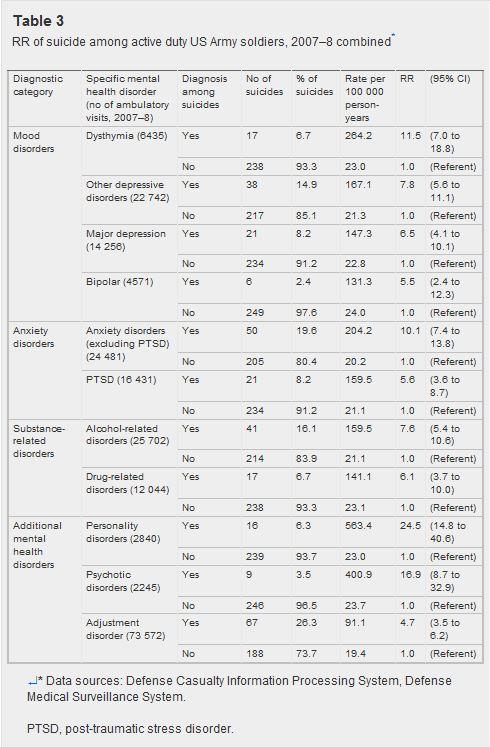
Among the anxiety disorders, soldiers with anxiety disorders other than PTSD had a RR for suicide of 10.1 (95% CI 7.4 to 13.8); those with PTSD had a RR of 5.6 (95% CI 3.6 to 8.7). Of the substance-related disorders, alcohol-related disorders had the strongest association with suicide (RR 7.6; 95% CI 5.4 to 10.6), followed by drug-related disorders (RR 6.1; 95% CI 3.7 to 10.0). The RR for suicide among those with personality disorders, psychotic disorders and adjustment disorder were also significant in comparison with soldiers without these diagnoses. It should be noted that rates for counts less than 20 are unstable; these rates should be interpreted with caution. This paper primarily examines the association of mental health risk factors with suicide among soldiers in the US Army. Mental health disorders, which are among the most consistently reported risk factors for suicide,8 ,10 have been shown to contribute to morbidity among active duty US military personnel.[37] Rates of suicide in the US Army increased more than 80% from 2004 to 2008. They thereby surpassed comparable civilian rates of suicide, which remained relatively stable during this time period. This increase, unprecedented in over 30 years of US Army records, suggests that approximately 40% of suicides that occurred in 2008 may be associated with post-2003 events following the major commitment of troops to Iraq in addition to ongoing operations in Afghanistan. The US Army population is predominantly male, young (<35 years old), and Caucasian (see Table 2). Consistent with the literature on civilian populations, this study found that male gender, younger age and Caucasian race were associated with higher rates of suicide.10 ,[38-40] Similar to previous findings in the US military, this study found that lower enlisted personnel have a higher rate of suicide.41 No association was found with marital status, potentially because long-term separations and overseas deployment may modify the protective effect of marriage that has been observed in civilian populations.[39 ,42-44] Suicide rates were higher among soldiers diagnosed with mental illness in the year before their suicide for all mental health disorders examined, findings that are consistent with studies in civilian and military populations.[9 ,12 ,21 ,23 ,24 ,45 ,46] Notably, over one quarter of soldiers who committed suicide had a diagnosis of adjustment disorder. Adjustment disorder, a relatively short-term diagnosis occurring in close proximity to stressful events, may be used when a more precise diagnosis has not been identified.[47] It is especially prevalent among military trainees[48-50] and in medical evacuation from combat theatre.[26] The overall rates of mental illness among active duty soldiers also nearly doubled since the major commitment of troops to Iraq and Afghanistan, mirroring the increase in rates of suicide from 2003 to 2008. This suggests a possible association between the increase in mental health disorders and suicide in a population under severe stress. The 2008 rate indicates that more than one fifth of all active duty soldiers had an ambulatory visit for a mental health disorder, implying a prevalent public health problem. The increase in suicide rates may be viewed as the tip of the ‘mental health iceberg’. While suicide remains a relatively rare event, its increase signals more prevalent underlying mental health problems among soldiers in the US Army. The parallel increase in trends of suicide rates and mental health disorders during the years 2003-8 suggests that army operations during this time period may have affected the nature and extent of mental health problems, including suicide. Earlier studies suggest that military deployment may increase the risk of mental disorders and psychosocial distress.[51-59] Given that current psychosocial stresses are thought to play a predisposing and triggering role in suicidal behaviour,[40 ,60 ,61] deployment and potential combat exposure may serve as a source of such stresses. Stress and potential risk factors for suicide, such as extended separations due to deployment and training, exposure to traumatic events in combat, homecoming issues, implications of legal difficulties for eligibility for re-enlistment and promotion, access to firearms, and weapons training may be especially relevant among military personnel.[62-64] The possibility of combat deployment as an effect modifier amplifying other risk factors should also be considered. In the present study, 31% of suicides were committed by soldiers who had never deployed, implying that psychopathology and stress other than combat exposure may contribute to suicide incidence in this population. Predeployment stress, such as anticipatory anxiety and preexisting trauma, may play an important role.[65-69] Changes in recruitment standards or screening processes before entrance into the army may also be involved. The role of non-combat stress in suicide incidence, as well as the effect of the increased pace of military operations throughout the army, need to be elucidated further.[70-72] Higher suicide rates among those with diagnosed mental health disorders suggest the importance of suicide prevention strategies, including identification, treatment and monitoring of major risk factors for suicide. Potential existing prevention strategies include: the education of ‘gatekeepers’ (such as clergy, primary care physicians and first responders) who have contact with populations vulnerable to mental health disorders and suicide;[73 ,74] effective treatment of depression and other mental disorders;[75 ,76] and proper gun storage practices.[77 ,78] All implemented policies, programmes and interventions should undergo ongoing evaluation, including existing army mental health and suicide interventions such as ‘Re-Engineering Systems of Primary Care for PTSD and Depression in the Military (RESPECT-mil)’, ‘Battlemind’ and ‘Ask, Care, Escort’ (ACE).[79-83] Surveillance of suicides and mental health disorders should continue to be routinely conducted to track trends and to monitor programme and policy effectiveness. LimitationsCounts of active duty soldiers with a primary diagnosis of a mental health disorder during 2007 or 2008 were used in risk calculations. Although persons with mental health secondary diagnoses may have been missed, using primary diagnoses provided certainty that the conditions were those for which the patient sought and received treatment. Relative rates may thus be conservative estimates. In most cases, however, the size and statistical strength of the relative rates strongly suggest an association with suicide. An additional limitation concerns the low counts of certain mental health disorders among the suicide cases. Caution must be used in interpreting these results, as such limited numbers result in unstable rate estimates and can easily underestimate or overestimate associations. Limitations of the DoD administrative, common-access databases from which the mental health data were obtained include the aggregated nature of the data, and that individual soldiers may have received assessment and treatment outside of the army medical environment (for which DoD databases would not have a record). For example, analyses do not capture mental health care received through alternative sources such as Military One Source or community health clinics.[84] The data also do not cover potentially relevant mental health diagnoses and treatment before enlistment in the army. Although the literature suggests that suicide results from multiple risk factors including personal stressors such as relationship, legal and financial problems,[41 ,85] this analysis focuses on mental health risk factors only. Furthermore, the study is limited in its ability to assess trends in association of mental health disorders with suicide over time because only associations for the period from 2007 to 2008 were examined. This study also does not assess the association of suicide with suicide attempts and suicide ideations. Finally, given the uniqueness of the military population, the generalisability of these results to other populations is limited. StrengthsThis analysis offers a preliminary epidemiological assessment of mental health risk factors for suicide among active duty US Army personnel using existing military medical surveillance and suicide report data. The results provide evidence of important mental health risk factors for suicide. Further exploration of these risk factors is needed. A particular strength of the present study was the reliance on data obtained from the Defense Medical Surveillance System, which encompasses all mental health medical encounters among active duty soldiers paid for by the US military health system, including care received in fixed military treatment facilities (ie, not temporary) as well as care received in civilian medical treatment facilities. In addition, suicide cases in the registry were obtained from official DoD and army casualty data sources (Defense Casualty Information Processing System, G1), in which reporting is generally complete. Whereas suicide counts are known to fluctuate slightly as cases are evaluated and re-evaluated, these counts are consistent with cases as defined in June 2010 when the data were obtained. Army suicide rates have been increasing since 2004, and rates of mental illness, indicators of soldier stress, have also been increasing during this same time period. A number of identifiable mental health risk factors were found to be associated with suicide in the US Army, including mood, anxiety, adjustment, personality, psychotic and substance-related disorders. The associations reported in this study are generally consistent with earlier research, but should be confirmed in studies with a longer time frame and a larger sample size. Future studies should use multivariate analyses to examine the effects of comorbid conditions and the relative contribution of multiple risk factors. Mood disorders, adjustment disorder, PTSD and alcohol-related disorders are of particular concern given their prevalence and strong association with suicide. The recent increase in suicide rates may be viewed as the tip of the ‘mental health iceberg’, signalling more prevalent underlying mental health problems. Before the increase in suicide rates, there was a slightly decreasing trend of suicide rates among active duty US Army personnel during the years 1977-2003, suggesting that the increase is associated with army operations subsequent to 2003. Further study is needed to define specific factors, both individual and social, which contributed to this increase. As risk factors for stress and mental health disorders, preparation for deployment and potential combat exposure may play an important role in these trends. Article Source: Injury Prevention 2012;18:405-412.
|
||||
|